Proctology
Haemorrhoids
What is Haemorrhoid/Piles?
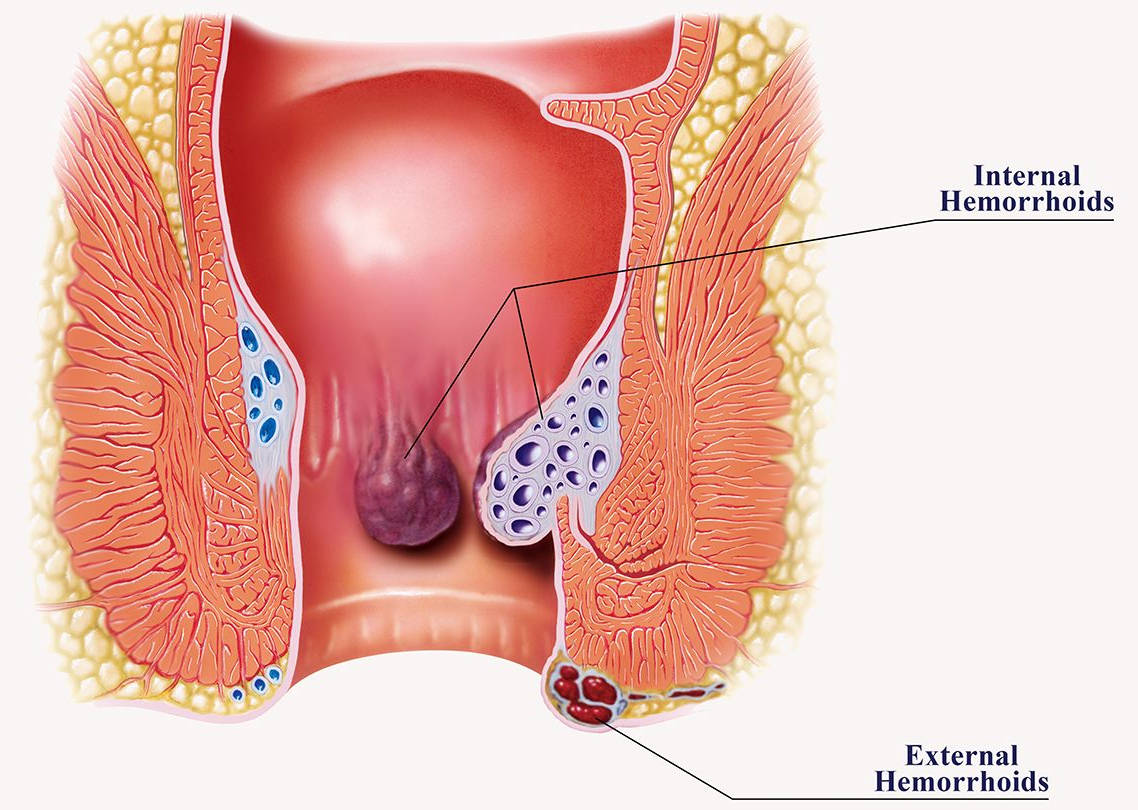
Haemorrhoids or piles are swollen/engorged veins in lower part of rectum/anal canal.
How will I know that I have haemorrhoids?
One of the most common concern for a visit to a surgeon is a bleeding pile. Patient either presents with bleeding which happens usually after passing motion and is described by the patient as a jet of blood, patient might notice blood while cleaning or in the pan. Many a times bleeding is not visible but over a period of time people develop anaemia.
Second most common presentation of a haemorrhoid is a mass protruding from the anus.
Depending on the stage the mass might come out while passing motion and it reduces back on its own, or it might come out and one is able to push it back or at times it stays out all the time.
If you have any of these symptoms you should consult a doctor who would do a local examination and might do a proctoscopic examination if you feel comfortable.

What are the treatment options for haemorrhoid?
Any treatment dealing with haemorrhoids should be targeted at dealing with the base of haemorrhoids and the hemorrhoidal pedicle where lies the feeding arterial supply of the haemorrhoid. Standard treatment involved tying the pedicle and excising the hemorrhoidal mass which led to formation of large wounds which took a long time to heal and were extremely troublesome for the patient.
Treatment evolved to stapler haemorrhoidectomy where a special single use device is used to deal with the base of haemorrhoid and staple the haemorrhoidal feeding vessels circumferentially. This is a good treatment option considering that there is no external wound, recovery is expedited and patient returns to work early with no frequent visits to the clinic. The only con being that it leaves behind a foreign body in term of staples and rarely might lead to infection, pain, or tenesmus later on. Improper technique might lead to a lower staple line which can be very painful. The only Achilles heel to this is recurrence. If patient is not very compliant or if the procedure is done early in life and later on there is recurrence the clinician is stuck with lack of alternate options.
DIODE laser effectively circumvents all these issues. It is effective in every grade of haemorrhoid. This treatment also does not leave behind any external wound and there is no frequent visit to the clinic. In addition it does not leave behind any foreign body hence negating the chance of complication associated with stapler and in the case of a recurrence the procedure can be easily repeated.
Traditional Haemorrhoidectomy

DIODE laser treatment for Haemorrhoids

I had pain/bleeding which was diagnosed as haemorrhoid but it resolved with medications. Now I don’t have any pain/bleeding. What should I do?
It is true that many times bleeding and pain of haemorrhoids resolves with medications. One must seek medical examination by a surgeon to assess the grade of haemorrhoid. Grade I and II haemorrhoids might be managed conservatively with medication but anything beyond that needs surgical intervention. If you leave the problem unattended gradually you might end up with complications.
What are the possible complications of hemorrhoids?
If untreated haemorrhoids will gradually enlarge and might come out of anal opening and become swollen and may not go back(prolapsed hemorrhoid).
There might be bleeding within the pile leading to a painful swelling(thrombosed pile).
You may develop anaemia due to persistent bleeding.
If I have the haemorrhoid surgery will it affect my digestion and do I need to be on lifelong dietary restrictions, will there be narrowing of anal canal, will I loose my ability to hold motions?
Haemorrhoids have no role in digestion as they are just a bunch of swollen blood vessels.
There are no specific dietary restriction but yes you would be advised to take healthy diet and avoid constipation.
With advancements in haemorrhoid surgery there is no risk of narrowing of anal canal and there is no change in ability to hold motions.
What are the preparations required before surgery and what should I expect during hospital stay and after discharge?
The preparation for surgery will be started from the outpatient department (OPD). You will be advised to undergo a few tests to assess your body functions and a pre-anaesthetic check-up (PAC) will be done by an anaesthesiologist (a specialist doctor) who will assess your fitness for anaesthesia.
Most likely you will be admitted on the day of surgery unless you have some specific concerns which warrant some extra stay before the surgery.
You will be advised not to eat or drink anything from midnight of the day prior to surgery and not to eat or drink anything on the morning of admission as well. If you take some medications regularly in the morning than please do not forget to discuss regarding them with your doctor so that he advices you on which medicine to take and which not to take.
Upon admission some paper work will be done and you will be asked to sign consent forms for anaesthesia and surgery.
You will be asked to change in to hospital clothing, shaving of the abdomen will be done and you will be given some intravenous medications and an enema.
Once the preparations are done you will be wheeled into the preoperative area where nursing staff and doctors will confirm your identity and then you will be shifted to the operating room.
Your anaesthetist will put you under spinal or general anaesthesia and then surgery will start. Usually it takes about one hour for the surgery to be over and then you will be shifted to post-operative recovery area in conscious state. You will be kept there for couple of hours and then you will be shifted to your designated room.
A catheter (pipe) might be put to drain out urine for maximum 24 hours and will be removed before you are Sent home.
You will be discharged to home the day after the surgery. You will be advised some medications on your discharge. You will be advised to take liquid diet at home for five days and then gradually you can start having normal diet.
Usually if all goes well you will be called for a visit to OPD five days after discharge.
How soon can I resume work after surgery? How much bed rest is advised? Is there any specific season of year when I should opt for surgery?
No bed rest is advised. You will be encouraged to walk about on your own from the next day of surgery. You can resume normal household work two days after surgery. Climbing stairs will not be a problem.
You may start driving one week after the surgery.
After a week you can resume walking. For a month you would be advised not to do weight training, running, jogging, cycling, yoga. You can resume all of this gradually after a month from the date of surgery.
Considering that almost all hospitals and households have air conditioning the season has become irrelevant so you can plan surgery as per the need and convenience anytime round the year.
