What is Obesity
Obesity is a chronic illness in which a person accumulates excess fat which can jeopardize health. The National institute of heath states that excessive weight becomes a health hazard when it is 20 percent or more above the ideal body weight, Anyone with a BMI of 30 or more is classified as obese.
Obesity is the result of an increase in the size or number of fat cells in the body. When a person gains weight, these fat cells grow in size and then in number. It can result in either significant physical disability or even death.
Obesity can be defined by the following criteria.
| Class | BMI(Global) | BMI(Indian) |
|---|---|---|
| Normal | 18.0-24.9 | 18-22.9 |
| Overweight | 25.0-29.9 | 23.0-27.9 |
| Grade I Obesity | 30.0-34.9 | 28.0-32.9 |
| Grade II Obesity | 35.0-39.9 | 33.0-37.9 |
| Grade III or Morbid Obesity | 40.0 and above | 38.0 and above |
Based on weight circumference:
| Increased risk to life | Substantial risk to life | |
|---|---|---|
| Men | ≥ 94 cms | ≥ 102 cms |
| Women | ≥ 80 cms | ≥ 88cms |
Obesity is more than a cosmetic issue
Obesity is a disease and a serious health risk
Many people have a misconception that being fat is simply a lack of self-control. Actually it is a complex syndrome that involves control of appetite and energy metabolism.
Similarly being obese is often mistakenly considered the same as being overweight. In clinical terms the difference is vital and often life threatening. Several medical organisations including WHO classify obesity as a disease and a serious threat to health.
Effect of obesity on various body systems
- Mechanical effects
– Hernia
– Gastroesophageal reflux disease
– Varicosities
– Joint problems
– Bony deformities
– Plantar fasciitis
– Gout and worsening of existing gout
– Obstructive sleep apnoea
– Hypertension - Metabolic Impact
– Diabetes mellitus
– Dyslipidaemia
– Polycystic Ovarian Syndrome
– Hypogonadism
– Cardiovascular issues
– Metabolic syndrome
– Deep Vein Thrombosis
– Stroke
– Thromboembolic episode
– Insulin resistance
– Infertility - Emotional and psychological impact
– Depression
– Loss of self esteem
– Workplace discrimination
– Lack of confidence - Impaired quality of life
Women and obesity
- Obesity, especially abdominal obesity, is central to the metabolic syndrome.
- Obese are particularly susceptible to diabetes.
- Diabetes, in turn, puts people at dramatically increased risk of cardiovascular disease (CVD).
- Those who are obese have a higher risk of low back pain and knee osteoarthritis.
- Obesity negatively affects both contraception and fertility as well.
- Pregnancy outcomes are negatively affected by maternal obesity (increased risk of neonatal mortality and malformations).
Childhood and Adoloescent Obesity
By 2025, India will have over 17 million obese children and stand second among 184 countries.
Children who are obese are five times more likely to develop in obese adolescents and hence obese adults.
Because of prevalent childhood obesity many diseases which were earlier seen in adults only, like diabetes, high blood pressure, joint destruction, reproductive disorders, high cholesterol, dyslipidemia and coronary artery disease, are now frequently diagnosed in childhood and adolescents.
Obese or overweight children often suffer from various psychological ailments as depression, low self-esteem and impaired quality of life.
Due to impairment of glucose homeostasis as a result of obesity these kids suffer from pancreatic beta cell exhaustion leading to early onset diabetes which is often misdiagnosed as Type I Diabetes.
The WHO commission on ending childhood obesity was established in 2014. The commission was tasked with producing a report specifying which approaches and combination of interventions are likely to be most effective in tackling childhood and adolescent obesity in different contexts around the world. The final report was submitted in 2016.
Key Recommendations
- Reduce risk of obesity by addressing critical elements in the life-course
- Tackle the obesogenic environment and norms
- Treat children who are obese to improve their current and future health
Multidisciplinary approach to losing weight
Obesity surgery is to be performed by surgeons specialised in obesity and laparoscopic surgery.
Because morbid obesity is a complex syndrome, it must be treated from several perspectives. Most obesity surgery units use a multidisciplinary approach. A team consisting of several types of professionals who are specialised in obesity and sensitive to the specific needs of morbidly obese patients are involved in activities such as:
- Evaluation of the patient prior to surgery assessing both the surgical alternatives and alternative treatments
- Providing training and treatment after surgery
- Dietary and psychological counselling
- Postoperative physical fitness program
- Long term follow-up and support required to maintain weight loss. At our institute we are happy to involve the primary treating physician of patients throughout the treatment.
Role of multidisciplinary team:
Doctors
Internal medicine specialist, endocrinologist/diabetologist, primary care physician, gastroenterologist and cardiologist:
- Coordination of patient care
- Check and treatment of obesity related medical problems
- Thorough physical and illness specific testing
Family Physician
- Evaluation of patient’s health condition
- Timely diagnosis of obesity and related diseases
- Guidance for the scientific way of treatment
- Post-operative assessment of the changes in the medical condition and treatment accordingly
Dietician
- Preoperative assessment of nutritional status
- Preoperative education on postoperative dietary and nutritional treatment(consistency, food product selection, portion size, meals, protein supplements, dietary supplements) as well as behavioural changes i.e. quality, quantity and technique of eating right. “obey your gut” is the key to success and needs to be taught to the patients.
- Follow up of dietary and nutritional treatment and behavioural changes during postoperative period
Psychologist/counsellor:
- Preoperative psychological evaluation with assessment of realistic expectations and insight into the life-long changes required in behaviour
- Early and continual postoperative follow-up
- Support and encouragement
- Assessment of emotional status
- Lifestyle changes
- Discussing reaction to the operation
Surgeon
- Preoperative assessment of the patient’s motivation and expectations
- Discussion of the benefits and risk of the different types of obesity surgery
- Choice of the operation best suited to the individual patient
- Postopeartive follow-up of the procedures performed
Physical Therapist
Proper guidance about the physical activities of the patient for fitness purpose.
INDICATIONS FOR BARIATRIC SURGERY
Is bariatric surgery the right solution for my patient?
- BMI >37.5 without presence of any obesity related co-morbidities or
- BMI > 32.5 with the presence of type 2 Diabetes / any obesity related co-morbidities
- Patients motivated to lose weight and commitment to long term follow up
- Patient should have attempted conservative methods of weight loss and failed
- Bariatric Surgery to be considered only between ages of 18 - 65 years
- Bariatric surgery may be considered in patients more than 65 years in the presence of severe obesity related co-morbidities / disability
- Bariatric Surgery may be considered in patients < 18 years in special situations after paediatrician / endocrinology certification , but after attainment of puberty or completion of skeletal maturity
OBSTRUCTIVE SLEEP APNOEA (OSA)
Obstructive sleep apnoea (OSA) is a disorder in which breathing is repetitively interrupted during sleep due to collapse of the upper airway. An apnoea is defined as complete cessation of breathing lasting 10 seconds or greater. OSA causes hypertension and neurocognitive impairment whilst severe OSA predisposes to coronary artery disease, stroke and increased mortality.
Signs and symptoms of obstructive sleep apnoea include:
- Excessive daytime sleepiness
- Loud snoring
- Observed episodes of breathing cessation during sleep
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty concentrating during the day
- Experiencing mood changes, such as depression or irritability
- High blood pressure
- Nighttime sweating
- Decreased libido
- As determined by Polysomnographic study ( Sleep Study )
- Obstructive events = hypopnea index (AHI) or respiratory disturbance index (RDI)
- Apnea-hypopnea index (AHI)The AHI is defined as the average number of episodes of apnea and hypopnea per hour.
- Respiratory disturbance index (RDI) Defined as the average number of respiratory disturbances (obstructive apneas, hypopneas, and respiratory event–related arousals [RERAs]) per hour.
- OSA severity is defined as
- mild for AHI or RDI ≥5 to <15,
- moderate for AHI or RDI ≥15 to ≤30,
- severe for AHI or RDI >30/h
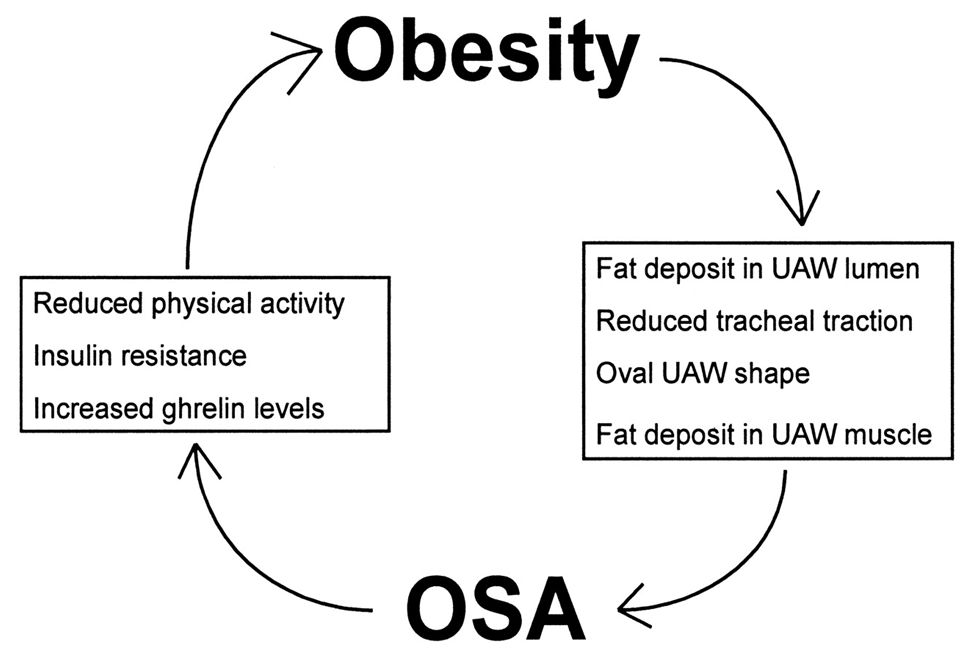
How is it related to Obesity?
- Obesity is the most significant predisposing factor for OSA.
- An elevation of 6 kg/m 2 in BMI leads to a four times greater risk of developing OSA.
- Central obesity, characterized by fat distribution at the abdominal level, upper body and neck, is the one most associated with OSA.
- Obese patients with OSA have 42% more fat in their neck, resulting in pharyngeal lumen narrowing and higher risk of OSA.
- Hormones produced by adipocytes, such as Leptin, are high in obese due to Leptin resistance. High leptin has a key role respiratory center control.
How to Diagnose – Screening
- STOP BANG score
- Snoring
- Tired
- Observed
- Pressure
- BMI
- Age
- Neck size
- Gender
- OSA - Low Risk : 2
- OSA – Intermediate : 3 - 4
- OSA - High Risk : 5 – 8
- or Yes to 2 STOP + male
- or Yes to 2 STOP + BMI > 35
- or Yes to 2 STOP questions + neck 17” /16”
Treatment options
Minimum 50% excess weight loss is the goal of treatment which can be achieved through various methods:
1) Supervised Diet and Exercise
2) Bariatric surgery
3) Patients with BMI >30 with a wide neck circumference and central obesity are the candidates for bariatric surgery
How does bariatric surgery help?
- Weight dependent benefits
– decreased mechanical force on the cervical region (pharyngeal lumen ), upper airway and diaphragm
– reduction in intra-abdominal pressure due to excess weight loss following surgery leads to a clinically significant improvement in blood oxygenation, resulting in favorable effects on the cerebral respiratory center - Weight independent benefits ( Metabolic )
- BRAVE
– bile flow alteration,
– restriction of gastric size,
– anatomical gut rearrangement and altered flow of nutrients,
– vagal manipulation and
– enteric gut hormone modulation. - Salutary effects of bariatric surgery are many, including improved mobility, agility, and physical endurance.
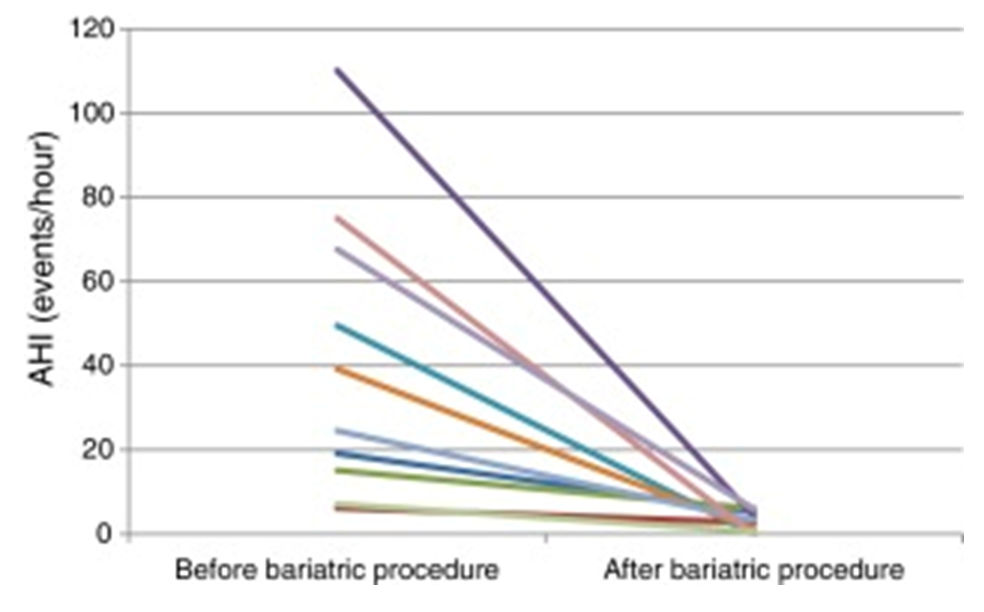
- Bariatric surgery results in dramatic reductions in BMI and apnea-hypopnea index.
Because obesity is a major predictive factor for OSA, weight reduction reduces the risk of OSA. The best data suggest that a 10% reduction in weight leads to a 26% reduction in the respiratory disturbance index (RDI). Benefits of weight reduction in include the following:
- Decreased RDI
- Lowered blood pressure
- Improved pulmonary function and arterial blood gas values
- Improved sleep structure and snoring
- Possible reduction of optimum CPAP pressure required
Weight gain is one of the most important determinants of relapse of OSA after surgical treatment. Although accomplishing and maintaining weight reduction are difficult, the results are extremely beneficial when patients can do so. The treatment approach is not complete if weight reduction is not addressed in patients who are obese.
Specific concern of OSA in Bariatric surgery and anesthesia
- Evaluation of systemic functions
- Metabolic evaluation
- Nutritional evaluation
Preparation phase minimum of five days up to three weeks for the obese as during this optimization towards the safety of anesthesia is achieved
POLYCYSTIC OVARIAN SYNDROME
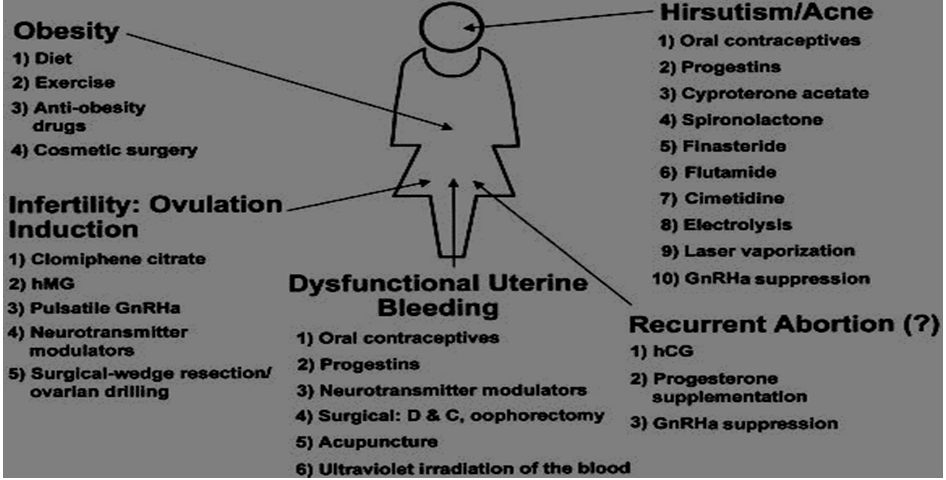
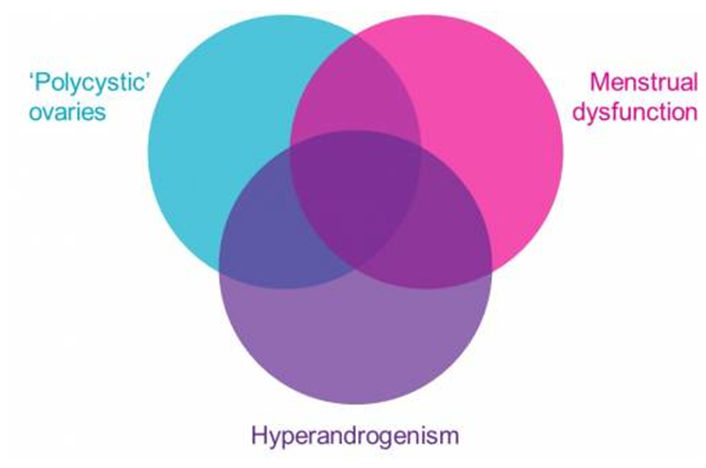
Polycystic ovary syndrome (PCOS) The original description given by Stein and Leventhal included obesity, amenorrhea, infertility and hirsutism in association with bilateral enlarged cystic ovaries showing a typical histological appearance of thickened capsule, multiple cysts and dense hypertrophied interstitial tissue.
It is a set of symptoms due to elevated androgens (male hormones) in women.
Signs and symptoms of PCOS include irregular or no menstrual periods, heavy periods, excess body and facial hair, acne, pelvic pain, difficulty getting pregnant, and patches of thick, darker, velvety skin. Associated conditions include type 2 diabetes, obesity, obstructive sleep apnoea, heart disease, mood disorders, and endometrial cancer.
- An exceptionally common disorder of premenopausal women.
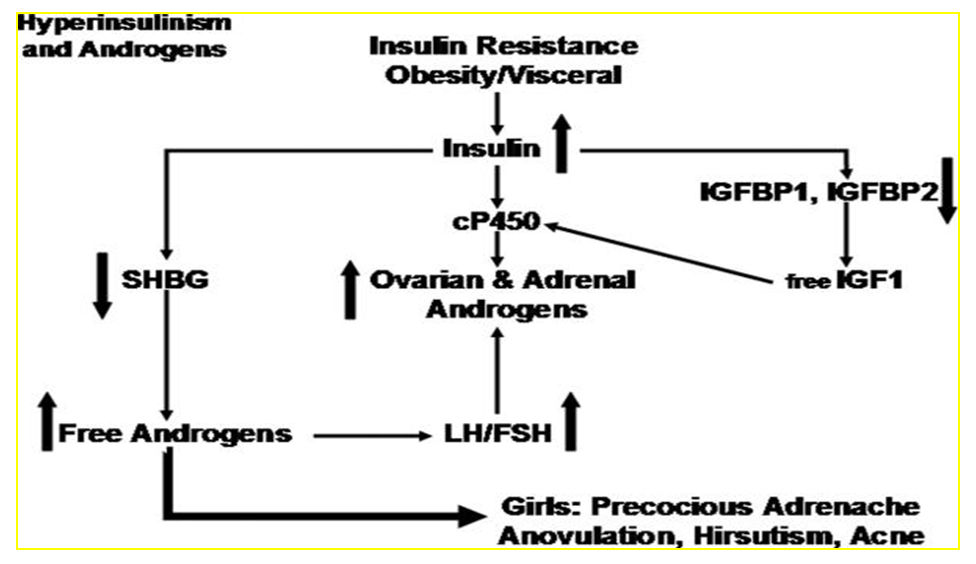
- INSULIN RESISTANCE is a common finding in PCOS.
| NIH Criteria | Rotterdam Criteria |
|---|---|
| Diagnosis requires both features: | Diagnosis requires 2 of 3 features: |
| Oligo and/or anovulation | Oligo and/or anovulation |
| Hyperandrogenism Clinical or biochemical | Hyperandrogenism Clinical or biochemical |
| - | Polycystic ovary morphology (Defined by at least one ovary demonstrating an ovarian volume>10 ml or presence of 12 or more follicles measuring 2-9 mm in size.) |
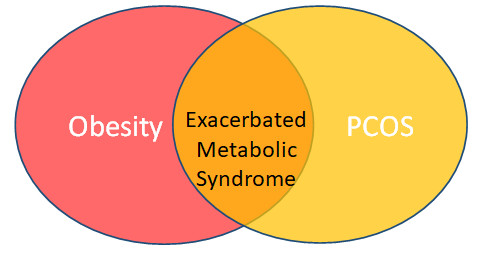
Role of obesity in PCOS
- Interestingly Obesity is not a part of the classification
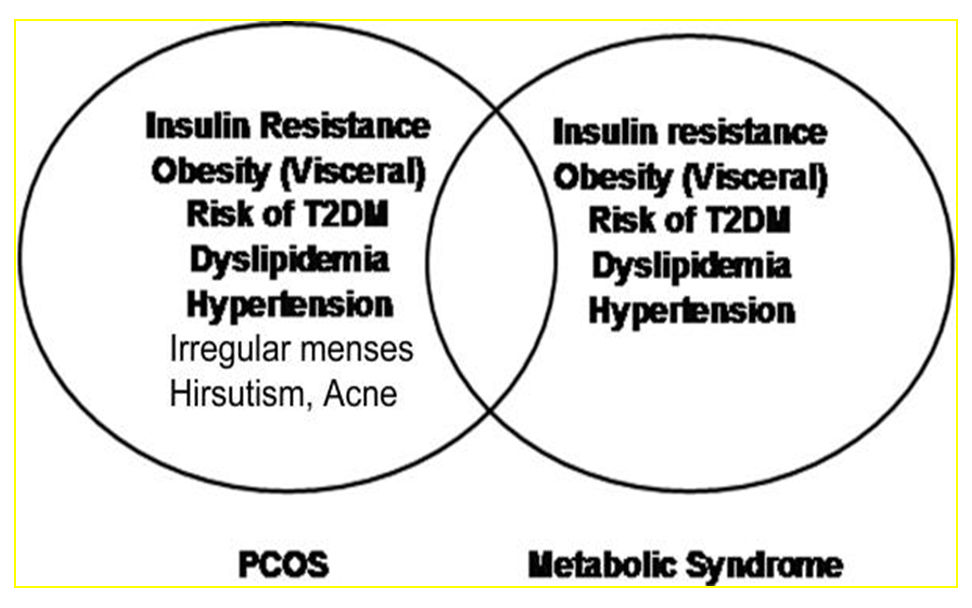
- However, obesity exacerbate many aspects of the phenotype especially T2DM, CV risk, Dyslipidemia.
- It adversely effects treatment of infertility and risk of pregnancy in those who conceive
Altered food preferences in PCOS
- Women with PCOS may have altered dietary consumption and food preferences
- Attributed to altered stress responses
- Associated with psychosocial problems, including depression, anxiety, chronic stress and reduced quality of life
Clinical manifestation Characterized by
- Polycystic ovaries
- Anovulation, infertility
- Menstrual irregularities
- Acanthosis nigricans
- Hirsutism, Virilization
- Obesity
- PCOS is a complex of physiological dysfunction produced by metabolic and hormonal factors
- Which with obesity predisposes to further complications like
- T2DM
- Endometrial hyperplasia and cancer
- Cardiovascular disease (CVD)
- Infertility & miscarriage,
- Social and emotional stress especially in adolescents
Insulin resistance and PCOS
Treatment for PCOS
There is a systematic algorithm to tackle various aspects of PCOS like hormonal, metabolic, infertility & virilization
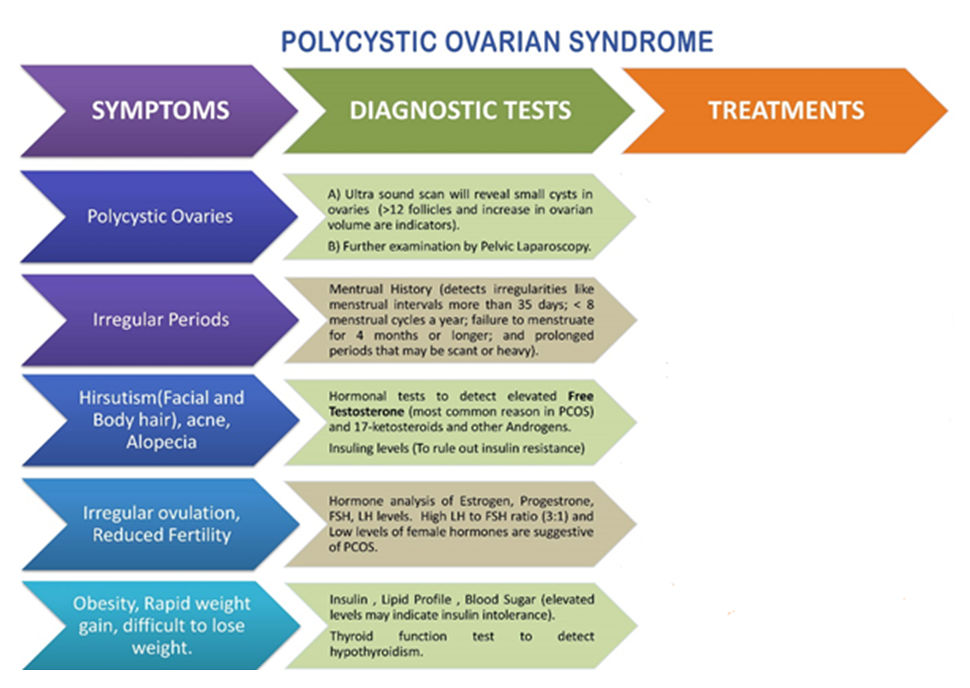
Polycystic ovary syndrome treatment starts with a proper diagnosis. Treatments are then chosen based on a woman's symptoms, age and future pregnancy plans. Treatment for PCOS is not effective unless the baseline metabolic disorders- Obesity and Insulin Resistance are dealt with scientifically.
Pathological and clinical tests for the Diagnosis of Obesity and Insulin Resistance:
- Blood sugar fasting and postprandial (Hyperglycaemia).
- Serum Insulin Fasting and postprandial (Hyperinsulemia).
- Lipid Profile (Dyslipidaemia).
- Fatty Liver on USG.
- Body Composition Analysis with fat % >30%.
- Body Mass index.
- Waist Circumference.
As per the scientific and clinical evidence, these are the treatments options for Obesity/Adiposity and the Insulin Resistance:
- Supervised Diet and Exercise Modifications are a must in this treatment. But may not be effective enough alone.
- Pharmacotherapy- Apart from Metformin and Orlistat, no pharmacotherapy in really available to treat adiposity/obesity/ metabolic syndrome. These two medicines have limited efficacy and may not help all.
- Bariatric Surgery in PCOS: Some scientific and evidence based facts:
10% of women worldwide are suffering from PCOS, and will seek help for gynaecological disorders or body image.
- Many women are at a risk of Metabolic Syndrome, predisposed to glucose abnormalities ie. DM, Dyslipidemia, Cardiovascular diseases.
- Metabolic consequences are grossly overlooked and undertreated.
- Metabolic syndrome and obesity co-exist.
- Bariatric surgery can be an effective and safe means of treatment for obese women with PCOS. Bariatric surgery can prevent or reverse Metabolic Syndrome associated with PCOS, leading to reproductive benefits.
- PCOS treatment requires combination of medical therapy, psychological support, lifestyle modifications and should include bariatric surgery as a firm treatment modality, wherever indicated.
- Benefits of Bariatric surgery include
- Achieve weight loss
Bariatric surgeries help obese women in terms of improved fertility index, improved Interpersonal relationships, improved sexual behaviour, prevention of Gestational Diabetes, & prevention of Pregnancy Induced Hypertension.
Women with morbid obesity, who are infertile secondary to PCOS, may have a new surgical option in the form of bariatric surgery.
Studies and research conducted report that 100 percent of the morbidly obese women who were diagnosed with PCOS-related infertility, and desired children, became pregnant within three years following Bariatric Surgery.
Metabolic improvements after bariatric surgery:-
- BMI and excess body weight decrease substantially after surgery.
- Improvement is noted in glucose abnormalities, dyslipidemia and hypertension.
- Improvement in diabetes mellitus and pre- diabetes status.
- Insulin abnormalities may improve very early post-operatively in pre-menopausal women with MS.
- Bariatric procedures, showed improved insulin values proportional to changes in BMI.
- The effects on hypertension have been shown to be independent of the magnitude of weight loss.
Evidence for surgery in PCOS patients:-
Reproductive age women fitting the profile of PCOS are included in many of the studies. Most women regained normal menstrual function and most had documented spontaneous ovulation. Patients had significant improvement in hirsutism, androgen profiles post Bariatric Surgery. Follow up for more than 2 years showed that all women resumed normal menstrual cycles, half had resolution of hirsutism and HbA1C decreased from 8.2% to 5.1%. Dyslipidemia, hypertension and diabetes mellitus almost completely resolved. Interestingly women became pregnant spontaneously after surgery.
78% of women saw improvement in metabolic syndrome and 48% showed improvement in PCOS specifically with regards to menstrual cycles, fertility and/or hirsutism.
PCOS presents a unique challenge since many obese PCOS women are adolescents. Although patients and physicians may at first be wary of a young patient considering surgical weight loss, these patients have an important opportunity. Bariatric surgery may actually provide primary prevention of coronary artery disease, eliminate MS and cause meaningful, long term reduction in morbidity and mortality. Young women with PCOS show evidence of atherosclerosis by abnormal carotid intimal medical thickness measurement and the prevalence of diabetes mellitus before the age of 50 is exceptionally high and estimated at 3-4 times the general population prevalence.
Reproductive considerations for bariatric surgery:-
Reproductive concerns may also lead PCOS women with MS to consider bariatric surgery. Does surgery optimize both fertility and pregnancy? The relationship between PCOS, obesity andinfertility has been documented for many years. Known effects include an ovulation, miscarriage, impairment in folliculogenesis and altered endometrial receptivity pregnancy. Risks in woman with MS are high. These women face difficulty in managing diabetes, pre-eclampsia, growth disorders, higher rates of caesarean delivery, higher maternal mortality and increase their children’s risks for metabolic disease in the future. Bariatric surgery in reproductive age women has been shown to decrease menstrual irregularities. PCOS women have less hyperandrogenism post operatively and sex hormone binding globulin increases after bariatric surgery. LH and FSH levels have been reported to increase after surgery. On a more functional level, ovulatory function measured by luteal LH and progesterone secretion improved postoperatively, although levels were still below normal expected values. Additionally, leptin levels decrease after bariatric surgery, reflecting improved reproductive metabolic status. Many of these women (10%-25%) have subclinical hypothyroidism which was significantly reduced following bariatric surgery. These changes certainly would suggest improved reproductive function.
Women already take pregnancy into consideration when electing for bariatric surgery. Although women tend to seek medical care for menstrual irregularities and hirsutism, this encounter offers a chance for testing, education and risk prevention of MS. Lifestyle modification and treatment of risk factors are appropriate and even necessary for long term control. Bariatric surgery is a powerful tool that should not be overlooked simply because a woman is young or presents with PCOS and MS rather than diabetes mellitus, myocardial infarction and severe chronic hypertension.
In our Experience of Bariatric surgery since 2003, we have treated more than 60% women patients for overweight/ Obesity and related co morbidities out of this population around 70% belong to the reproductive age.
The BMI range was between 28 to 70 kg/m2. 42% of these had come with the PCOS and infertility as the primary concern. All of them shod improved ovulatory function and fertility index after Bariatric surgery.
We have been following them regularly and been the International Centre of Excellence we provide the allied complete support.

HYPERTENSION
- HTN is most important risk factor for premature cardiovascular disease
– more common than cigarette smoking, dyslipidemia, and diabetes. - HTN accounts for an approx. 54 percent of all strokes and 47 percent of all ischemic heart disease events globally*.
- The increase in CV risk occurs with:
– Elevated systolic pressure in more than age 60 years
– Elevation in diastolic pressure in younger individuals.
– Elevation in Pulse pressure (large artery stiffness)
Benefits of reducing BP - A 10 - 12 mmHg reduction in SBP and a 5-6 mmHg reduction in DBP can potentially cause:
– 38% reduction in risk of stroke
– 16% reduction in risk of coronary disease*.
HTN & Metabolic syndrome - There is a substantial interconnection between metabolic factors and hypertension, beyond what we comprehend at the moment.
- Among nondiabetic hypertensive patients, poor BP control is associated with two fold increased risk of diabetes**.
- Diabetic patients may require more intense treatment to achieve the same blood pressure levels as nondiabetic individuals
Obesity & HTN: - Insulin Hypothesis
- Metabolic syndrome of central, or android, obesity leads to the development of HTN via:
– insulin-induced sodium reabsorption
– increased catecholamine sensitivity. - However, it is possible that insulin resistance and hypertension simply coexist in centrally obese subjects without a specific causal relationship.
- In many studies, HTN in severely obese patients was not associated with hyperinsulinemia.
- Increased intra-abdominal pressure, as seen in central obesity, is the cause of systemic HTN through three mechanisms*:
– increased renal venous pressure leading to activation of the RAA system, with resultant glomerular capillary injury and proteinuria;
– direct renal compression with activation of the RAA system;
– Increased intrathoracic pressure leading to a decreased venous return and cardiac output with further activation of the RAA system. - The net effect of these physiologic perturbations is:
– sodium and water retention,
– increased blood pressure,
– proteinuria
Effect of Bariatric Sx on HTN - Systematic review
- 31 prospective and 26 retrospective studies evaluated
- A total of 96,460 patients were evaluated; 52,151 had HTN prior to surgery.
- Overall, HTN resolved in 50% and improved in 63.7%.
- Sugerman et al* reviewed 1,025 patients out of which 51% had HTN
- At 1 year, patients had 35 ± 9% WL.
- HTN resolved in 69% and diabetes in 83%.
- Patients who resolved their HTN had greater %WL.
- At 5-7 years after RYGB (50% follow-up), %WL was 31 ± 13; resolution of HTN was 66% and DM 86%.
Meta-analysis with 1-2 yr FU - 19 papers, 6,587 subjects, 1-2 year FU
- There was a rapid reduction in the risk of hypertension as BMI decreased by up to 10 units, followed by a slight increase.
- Better resolution of HTN with RYGB / BPD vs. AGB
Meta-analysis with 5 yr FU - 22 papers, 4,160 subjects
- Reduction in the risk of HTN plateaued about 20 months after surgery,
- Reduction in the risk of DM and hyperlipidemia continued for a further year before levelling off.
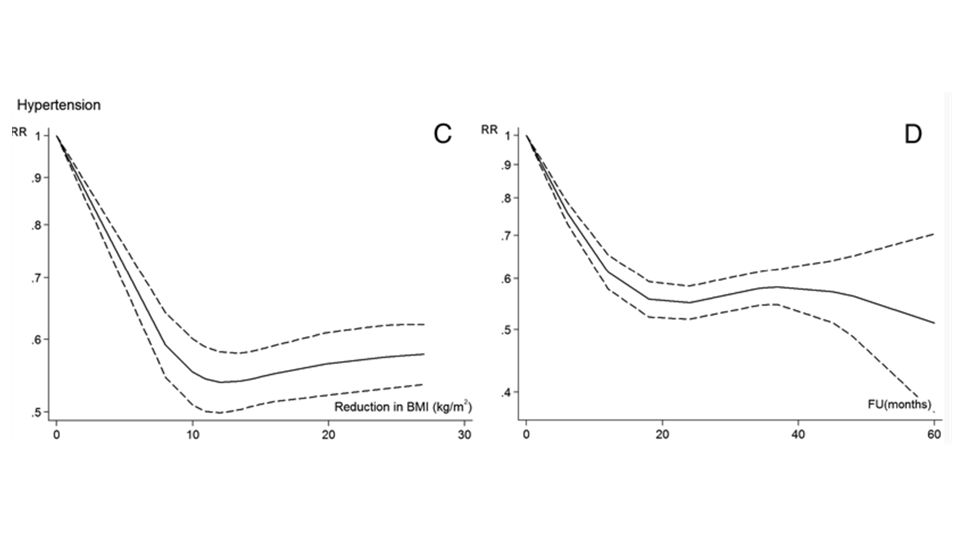
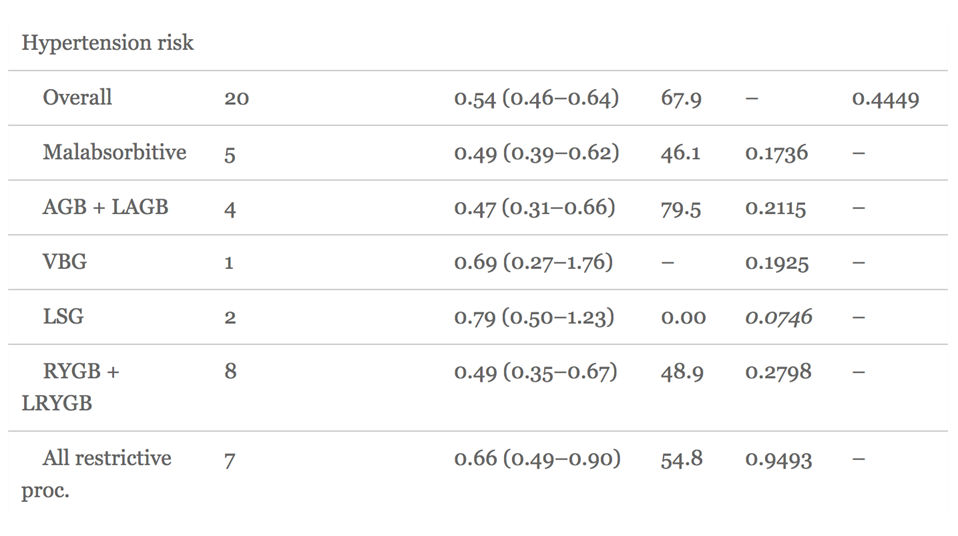
Conclusions
- Bariatric surgery leads to significant improvement in HTN
- Reduction of BP significantly reduces CV risk
GERD
GERD is a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications
Characteristic symptoms of GERD are retrosternal burning (often labeled as heartburn) and regurgitation.
The most common manifestation of esophageal injury is reflux esophagitis
GERD and Obesity-Association
- Obesity is a risk factor for gastroesophageal reflux disease (GERD)
- Approximately 50% of morbidly obese patients have GERD
- Meta-analyses have shown a positive correlation between the 2 conditions
- Obesity (BMI>30 kg/m2) significantly increased the likelihood of suffering from GERD.
- Obese people were almost 3X as likely to suffer from GERD as those with normal weight (BMI<30 kg/m2).
PATHOPHYSIOLOGICAL DISTURBANCES IN OBESITY
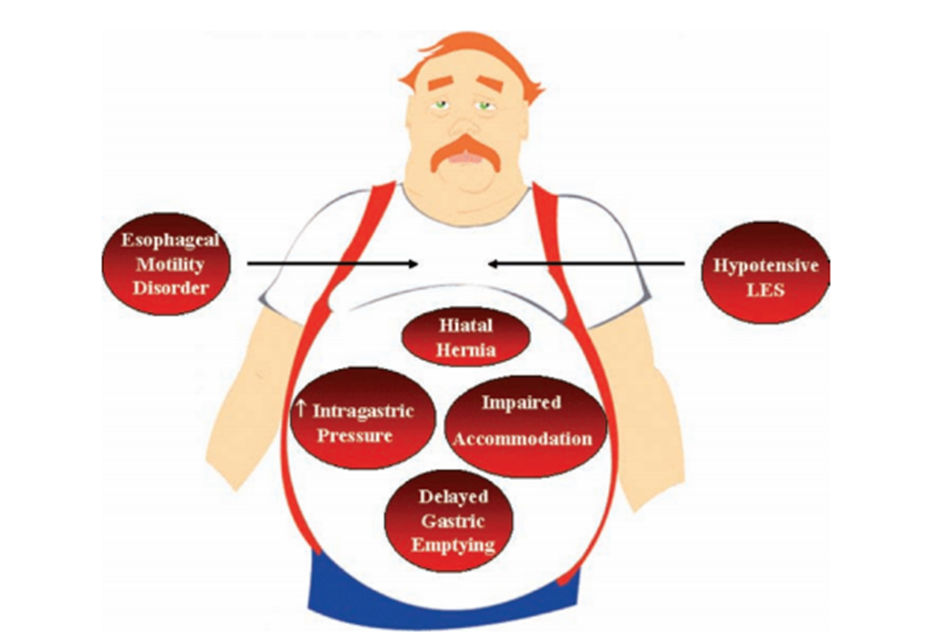
Mechanism of GERD
- LES - mediastinal position and/or with a short intraabdominal length
- A low resting LES pressure
- Transient relaxation of the LES
- Increased intra-abdominal or intragastric pressure
- Decreased esophageal clearance
- Anatomic abnormalities - HH
ROLE OF SEVERE OBESITY IN GERD PATHOPHYSIOLOGY
43 consecutive severely obese patients with 53 normal people were compared in one study
- lower LESP
(11.9 ± 5.3 mmHg vs 15.9 ± 2.7 mmHg) - 51% were noted to have abnormal acid exposure
- TLESR - increased frequency
7.3 ± 2.0 events/2 h vs 2.1 ± 1.2 events/2 h compared to normal individuals, - crural diaphragm inhibition,
- esophageal shortening
- positive pressure gradient between the stomach and the gastroesophageal junction
Why Bariatric Surgery
Significant reduction/ amelioration of GERD symptoms:
- medication utilization reduced
- weight reduction along with resolution of comorbidities
Recommendations-SAGE:
Due to concerns for higher failure rates after fundoplication in the morbidly obese patient (BMI >35 kg/m2) and the inability of fundoplication to address the underlying problem (obesity) and its associated comorbidities, gastric bypass should be the procedure of choice when treating GERD in this patient group (Grade B).
During operations for Roux-en-Y gastric bypass, sleeve gastrectomy and the placement of adjustable gastric bands, all detected hiatal hernias should be repaired.
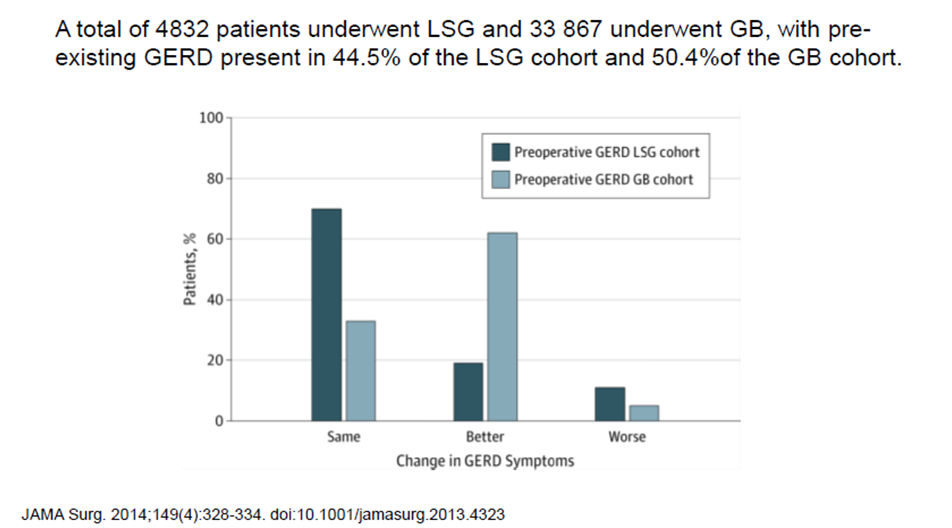
Conclusions-LSG and GERD
- There appears to be a slight trend towards an increased prevalence of GERD symptoms following LSG, but due to the suspected high heterogeneity in the literature, no definitive conclusion can be made.
- Objective esophageal function tests, with 24-hr pH studies being the ‘gold standard’, appear to report paradoxical results, making it impossible to determine the exact effect of laparoscopic SG on the gastroesophageal function.
- New-onset GERD symptoms and pathologic 24-hr pH results are reported however, including in studies reporting an overall decrease in prevalence of GERD following laparoscopic SG
- Standardization of the technique in terms of bougie size, concomitant HHR and the angle under which to staple of the fundus when performing laparoscopic SG is must.
- Further prospectively designed studies using both standardized questionnaires and objective esophageal function tests are needed to provide a definitive answer to this important question.
- Since there is a paucity of these studies, and with the knowledge that new-onset GERD symptoms are a relatively frequently described phenomenon.
RYGB in Morbidly obese for GERD
- The most effective bariatric procedure in the alleviation of GERD appears to be RYGB, which has been reported to have a similar efficiency as that of Nissen fundoplication.
- RYGB provides the best alleviation of symptoms associated with GERD and its comorbidities.
CONCLUSIONS
- Adequate study of patient’s symptoms must be made. An exhaustive patient selection is important for having good outcomes
- Methodical and standardized surgical technique is the key to avoid complications.
- Always look for a hiatal hernia and fix it.
DIABETES
Diabetes Severity Score
| Score | ||
|---|---|---|
| Parameters | 1 | 2 |
| Age (Years) | 30-60 | > 60 or < 30 |
| BMI (Kg/ m2) | >27 | ≤27 |
| Duration of Diabetes (Years) | < 10 | ≥ 10 |
| Microvascular involvement (Nephro/Retino/Neuropathy) | Absent | Present |
| Macrovascular involvement (Cardio/Cerebro/Peripheral Vascular) | Absent | Present |
| Mandatory insulin usage | No | Yes |
| Stimulated C- peptide (ng/ml) | ≥ 4 | < 4 |
Grading the Severity
Grade I = Mild / ‘Favourable’ diabetes-- score 7-8
Grade II = Moderate 9-11
Grade III = Severe diabetes -- 12-14
METABOLIC SURGERY
From the Triumvirate to the Ominous Octet: A New Paradigm for the Treatment of Type 2 Diabetes Mellitus
- Inadequate insulin release from beta cells, disrupted early phase insulin effect
- Insulin Resistance (IR) in peripheral tissues
- Increased endogenous glucose production (hepatic / intestinal glucose output)
- Adipocytes (accelerated lipolysis)
- Gastrointestinal tract (incretininsufficiency / resistance)
- Alpha cell (hyperglucagonemia)
- Kidney (glucose reabsorption)
- CNS (insulin resistance - others)
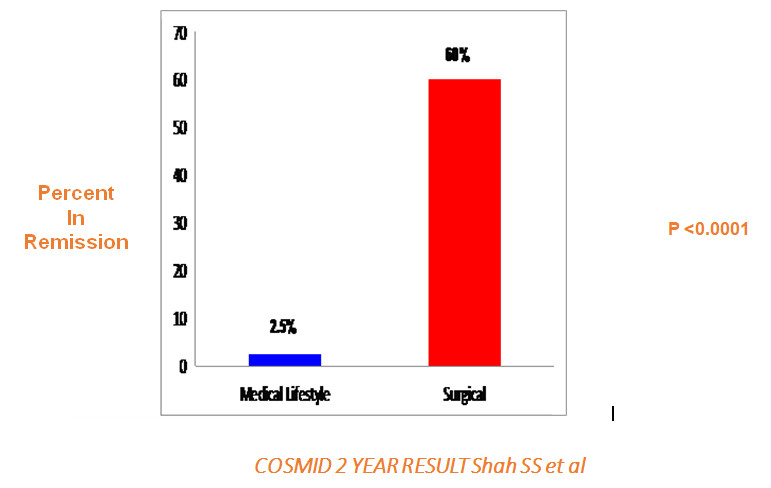
Bariatric Surgery
- It can improve T2DM in 90% of patients by:
1. Lowering blood sugar.
2. Reducing the dosage and type of medication required.
3. Improving diabetes-related health problems. - It can cause T2DM to go into remission in almost 78% of patients by:
1. Reducing blood sugar levels to normal levels.
2. Eliminating the need for diabetes medications.
Definition : DM Remission
- Glycated haemoglobin (HbA1c) <6% without hypoglycemic medication at 1 year (Fasting glucose below 7 mmol/L 2 hour glucose after OGTT <11.1 mmol/L)
- Partial Remission HbA1c <6.5%
- Glycemic control HbA1c <7 without OHA
Types of bariatric surgeries and their effect on DM (remission rate)
* 3 types:
- Restrictive procedure: Adjustable gastric band (AGB) and sleeve gastrectomy (SG).
- Malabsorptive procedure: Biliopancreatic diversion (BPD) and biliopancreatic diversion with duodenal switch (BPD-DS).
- Mixed procedure: Roux-en-Y gastric bypass (RYGB).
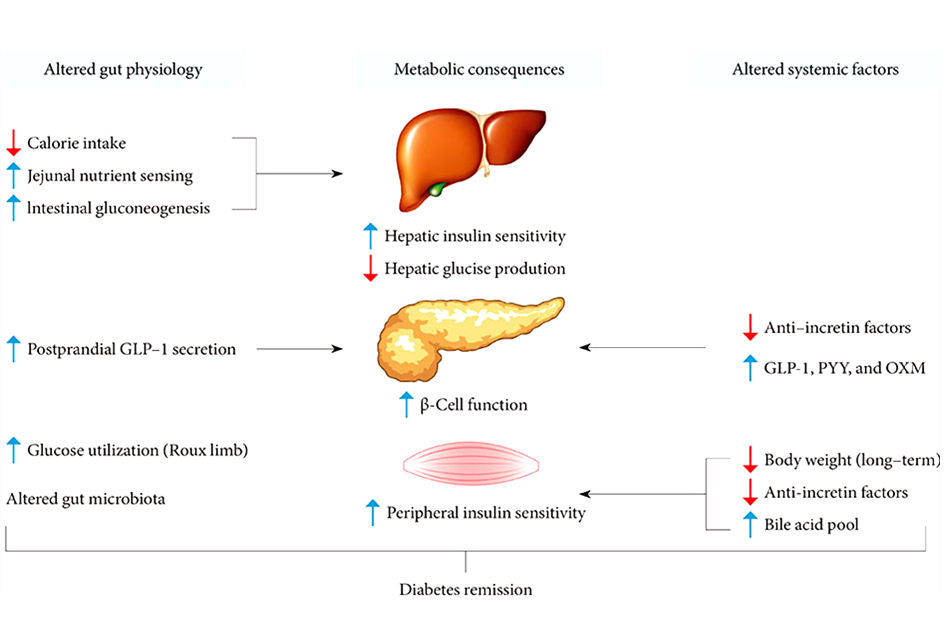
Mechanisms of Action
Hypothesis
- Caloric Restriction
- Ghrelin Reduction
- Foregut – Diversion of food
- Hindgut -- Incretin stimulation
- Others Bile Acids, Microbiota
- SG….Caloric restriction + Ghrelin Reduction + Rapid transit Incretin response + weightloss (better insulin sensitivity) + fatty liver correction (improved hepatic insulin sensitivity)
- RYGB – Above + Diversion from duodenum + Faster incretin response
- MGB – ALL + FASTER Ileal Stimulation
- BPD-DS – ALL + EVEN FASTER Ileal Stimulation
Primary Endpoint: Diabetes PARTIAL Remission at 2 Years
(HbA1c ≤6.5 Off All Diabetes Medications)
Remission of Type 2 Diabetes after Bariatric Surgery in Obese
| Procedure | Remission ( % ) |
|---|---|
| Vertical banded Gastroplasty | 75-83 |
| Laparoscopic adjustable silicone Gastric Banding | 40-47 |
| Roux-en-Y Gastric Bypass | 83-92 |
| Bilio-pancreatic diversion/ DS | 95 - 100 |
Resolution of DM after bariatric surgery in Indian patients
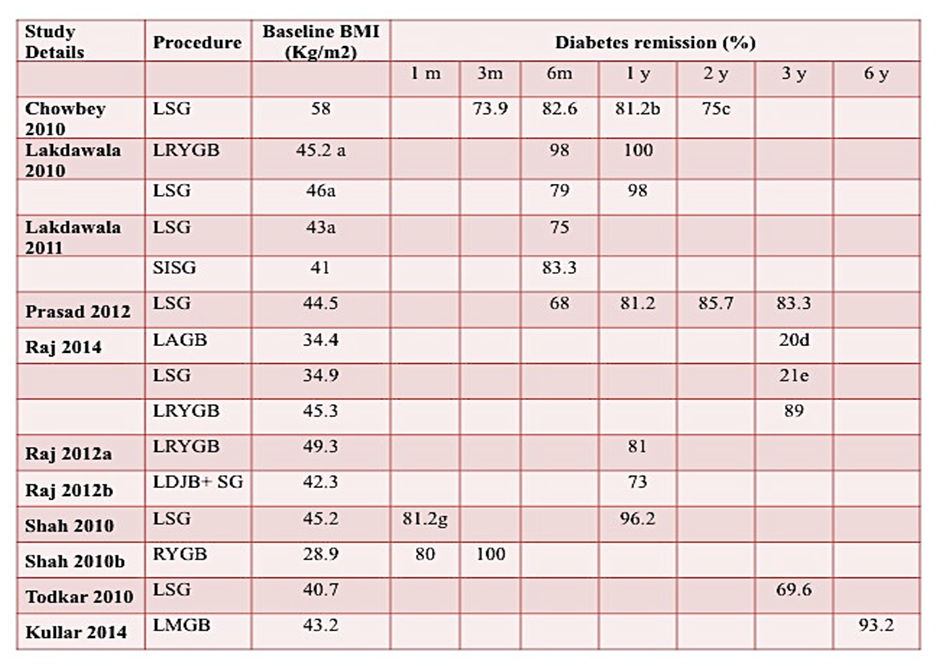
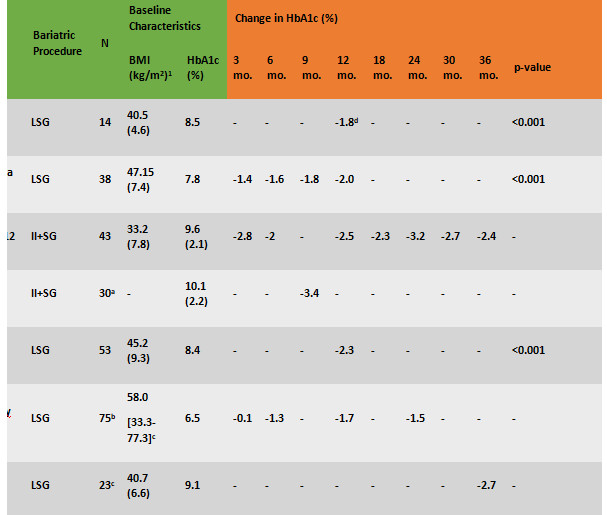
HbA1c outcomes in Indian patients following bariatric surgery

Leave a Reply